Is Cannabis safe for your heart? Here’s what we know so far.
As cannabis use expands in the U.S, investigating its effects on health is more important than ever. Recently, studies have raised important questions about cannabis’ impact on heart health. Can cannabis contribute to heart disease, stroke, or other cardiovascular problems? And how can people use it safely?
What research suggests
Over the past few years, a pattern has been catching researchers’ attention, studies suggest that people who use cannabis, especially regularly or heavily, might be facing a higher risk of heart-related problems.
In 2025, a meta-analysis of 24 studies reported that cannabis users had about a 29% higher chance of having serious cardiovascular events like heart attacks or strokes. That doesn’t mean cannabis directly causes these problems, science rarely works in absolutes, but it’s a signal we can’t ignore.
A 2024 study in the Journal of the American Heart Association took a closer look at survey data from across the U.S. and found a clear trend: the more days per month someone used cannabis, the higher their risk of heart issues. Heavier use seemed to carry a heavier risk.
Then, one of the largest retrospective studies to date analyzed the medical records of over 4.6 million people, all under age 50, following them over three years. They found that cannabis users had a sixfold increase in heart attack, a fourfold increase in ischemic stroke, a twofold increase in heart failure, and a threefold increase in cardiovascular death, compared to non-users. In 2025, a study in JACC Advances found similar links between cannabis use and acute heart problems, with younger users appearing especially at risk.
In another study from UCSF, researchers looked at 55 healthy cannabis users, some who smoked and others who used edibles, and compared them to non-users. They measured something called vascular function, how well the blood vessels can relax and expand. That ability is crucial for regulating blood flow and blood pressure, and when it’s impaired, it’s an early sign that the cardiovascular system may be under stress. This study showed that vascular function in cannabis users was about half that of nonusers. And here’s what’s really interesting, only the smokers showed harmful changes in blood markers related to inflammation and blood vessel injury. That suggests that smoking adds a layer of risk beyond THC itself.
These findings suggest that cannabis use, especially frequent or higher-dose use, might be associated with increased risk of cardiovascular events or vascular dysfunction.
Cannabinoids and the heart
Our bodies make their own cannabinoids, chemicals that help control things like inflammation, blood pressure, and how blood vessels behave. Cannabis interacts with that system, especially THC, the substance that causes the “high”. It can make the heart beat faster and the blood pressure go up. That pushes the heart to work harder, which may be a problem if someone already has narrowed arteries or other conditions. It can also cause blood vessels to tighten, which might reduce flow in sensitive areas like the heart or brain. Over time, THC may trigger inflammation and damage in the vessels.
CBD on the other hand, doesn’t bind to the same receptors as THC and may even help with relaxing vessels or lowering inflammation according to some lab studies. But we don’t know yet if it has the same effect in humans.
We know even less about other minor cannabinoids and terpenes, the aromatic compounds that give the plant its scent. These chemicals might have their own effects on the heart and blood vessels, but the science on that is still in its early days.
The key thing to understand is that cannabis isn’t just one drug. It’s a mix of different active compounds and they don’t all work the same way. Some may affect the cardiovascular system more than others, and possibly in opposite directions.
What we don’t know
Let’s talk for a minute about what this research does not actually show. In science, it is just as important to know the limits of the evidence as it is to focus on the results.
Right now, most of what we know about cannabis and heart health comes from what’s called observational studies. That means researchers are looking at people’s real-life behavior and health without trying to control who uses cannabis or how much they use, just observing people’s choices and outcomes. These studies are especially important for discovering associations and patterns to help researchers decide where to look more closely next.
They help us see when certain exposures, like cannabis use, tend to show up more often alongside specific health outcomes, like heart disease or stroke.
So, observational studies can tell us if two things tend to go together, but not if one is causing the other.
Other factors, like diet, exercise, stress levels, or even use of other substances, might be driving some of the risk we see. Additionally, most of the data we have so far comes from younger adults, so we don’t yet know what these risks look like in older adults or in people who already have cardiovascular disease, who might be most vulnerable.
Clinical trials are usually the gold standard to obtain evidence of cause and effect when testing new treatments before being launched to market. For cannabis, running large clinical trials is tough when regulations get in the way. Another thing to consider is that cannabis is already being used every day, in so many different forms, that a tightly controlled trial often can’t capture real-world patterns very well. In that sense, studies more similar to “phase 4” drug research, which track safety and effectiveness once a product is already in use, may be more appropriate for understanding cannabis.
Real-World Cannabis use and heart health
One of the biggest roadblocks in cannabis and heart research is knowing what people are using. Most studies rely on patients’ self-reported cannabis use and broad categories, like “ever used” or “used in the past 30 days.” That leaves out important details like how much THC someone used, how often, in what form, and how their habits changed over time.
Cannabis dispensaries already track a lot of this information through point-of-sale systems. Every purchase comes with a record of product type, THC, CBD, and other cannabinoids content, how much was bought, and when. If researchers could securely and ethically link that purchase data with patients’ health records, while protecting privacy, we could finally answer questions that so far have been out of reach: How does risk increase with higher doses or stronger products? Are edibles safer than smoking? Is there a threshold where risk starts to climb? Could we even monitor which strains or product lots are tied to more side effects?
This kind of approach could remove one of the biggest blind spots in cannabis research, bringing us closer to giving people real, practical guidance based on how cannabis is used in the real world.
Management Science Associates, a data analysis company based in Pittsburgh, has been working on this. Since 2017, they’ve been collecting and analyzing cannabis sales data from several states, linking product details with health data. This approach could enable researchers to produce studies precise enough to understand cannabis risks and safety and provide clear health and policy guidance.
The team used this very approach in a study to explore how real-world cannabis use relates to heart health, linking cannabis purchase data with electronic health records. The study included over 3,200 adults, compared cannabis users with non-users, and looked at both younger adults (ages 20–39) and older adults (ages 40–79).
Here’s what this study found:
- In older adults, cannabis use did not raise the 10-year risk of cardiovascular disease. Age, diabetes, and being male were much stronger predictors of risk than cannabis itself.
- In younger adults, cannabis use was linked to higher odds of being in the high-risk group for lifetime cardiovascular disease. Higher body weight also played a role.
- When examining risk markers, cannabis users tended to have slightly lower blood pressure, a lower LDL, often labeled “bad” cholesterol, and higher HDL, commonly referred to as “good” cholesterol.
That might seem like a protective effect, but it’s important to remember that LDL and HDL are no longer viewed as entirely “good” or “bad” in isolation. Research suggests it’s the quality and function of these lipoproteins, not just how high or low their levels are, that matter most for cardiovascular risk.
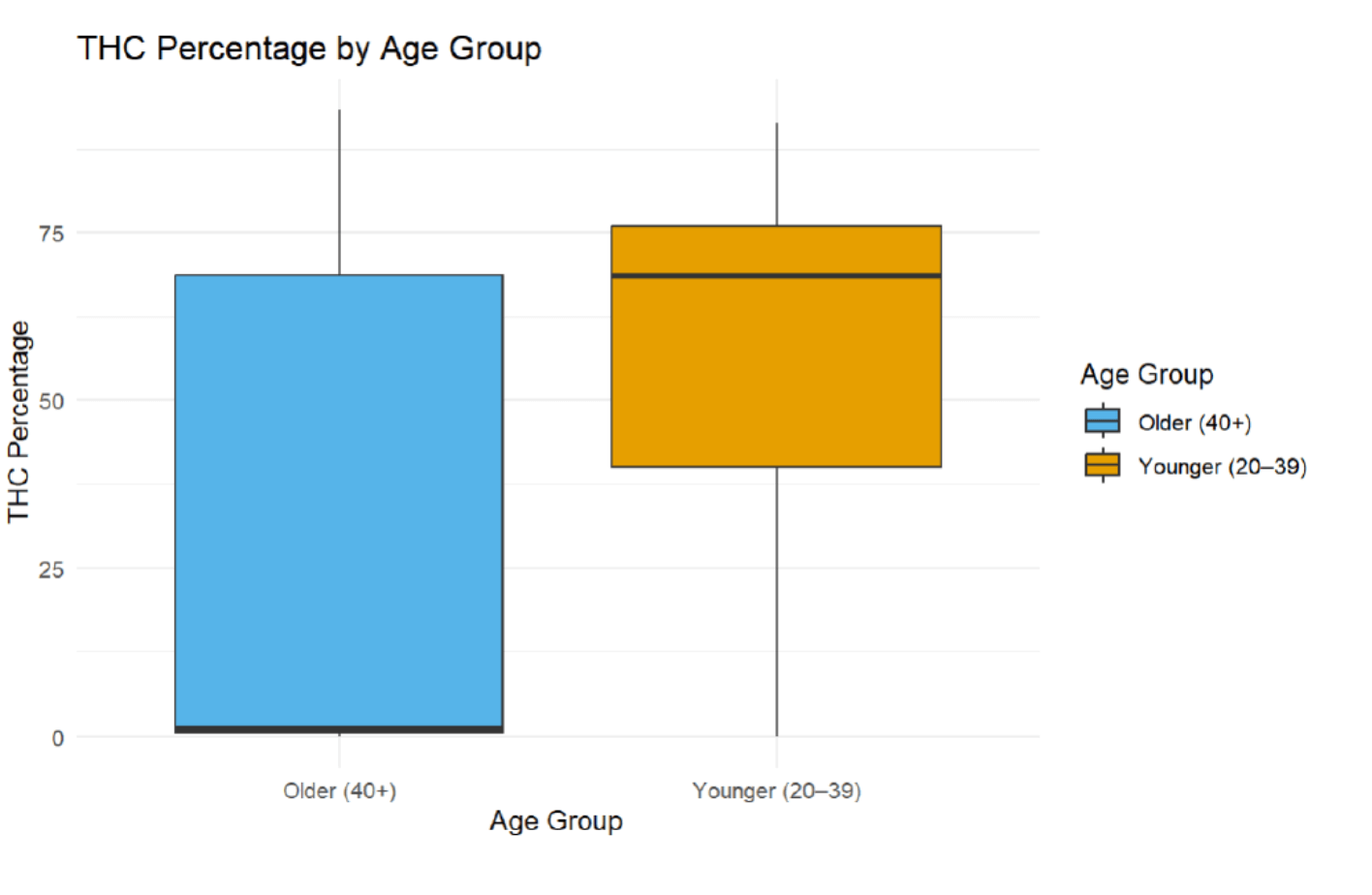
- Younger patients were consuming products with higher THC percentage than patients in the older group.
- Edibles and capsules looked safer in older adults, while vapes stood out as riskier across both age groups.
- THC and CBD seemed to pull in different directions. Higher THC levels were tied to higher cardiovascular risk, while higher CBD levels leaned toward lower risk.
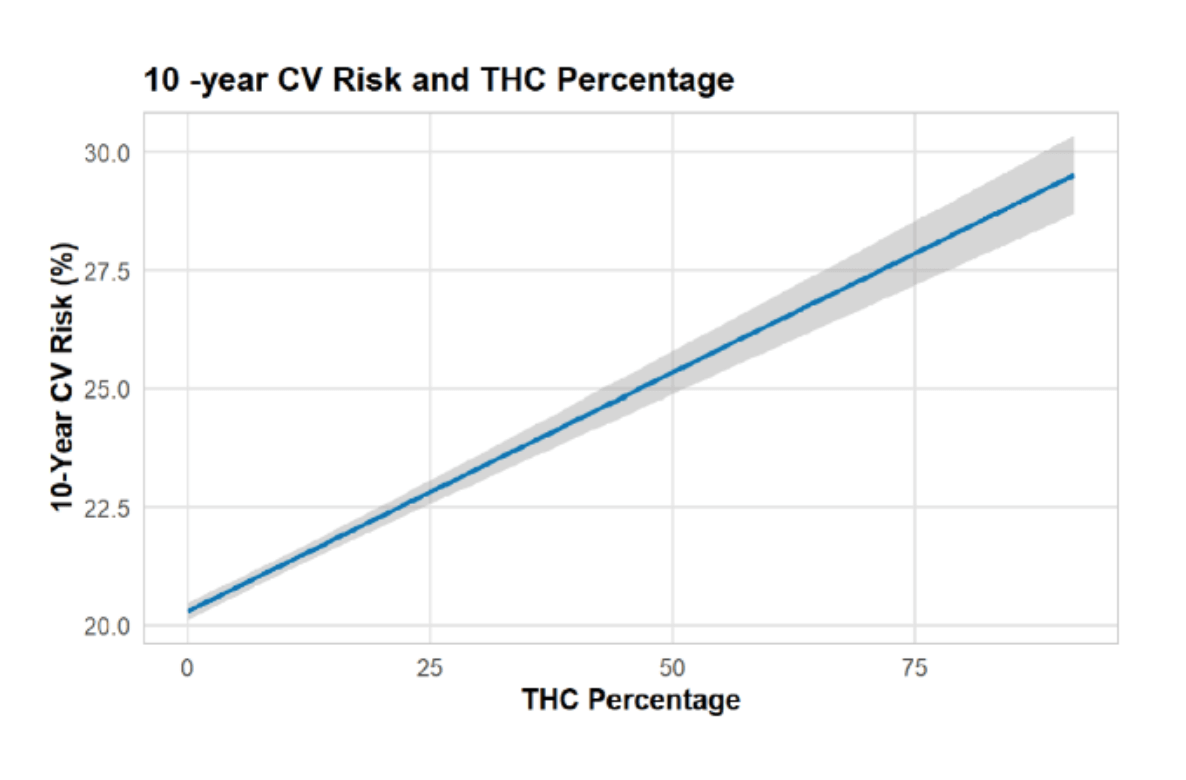
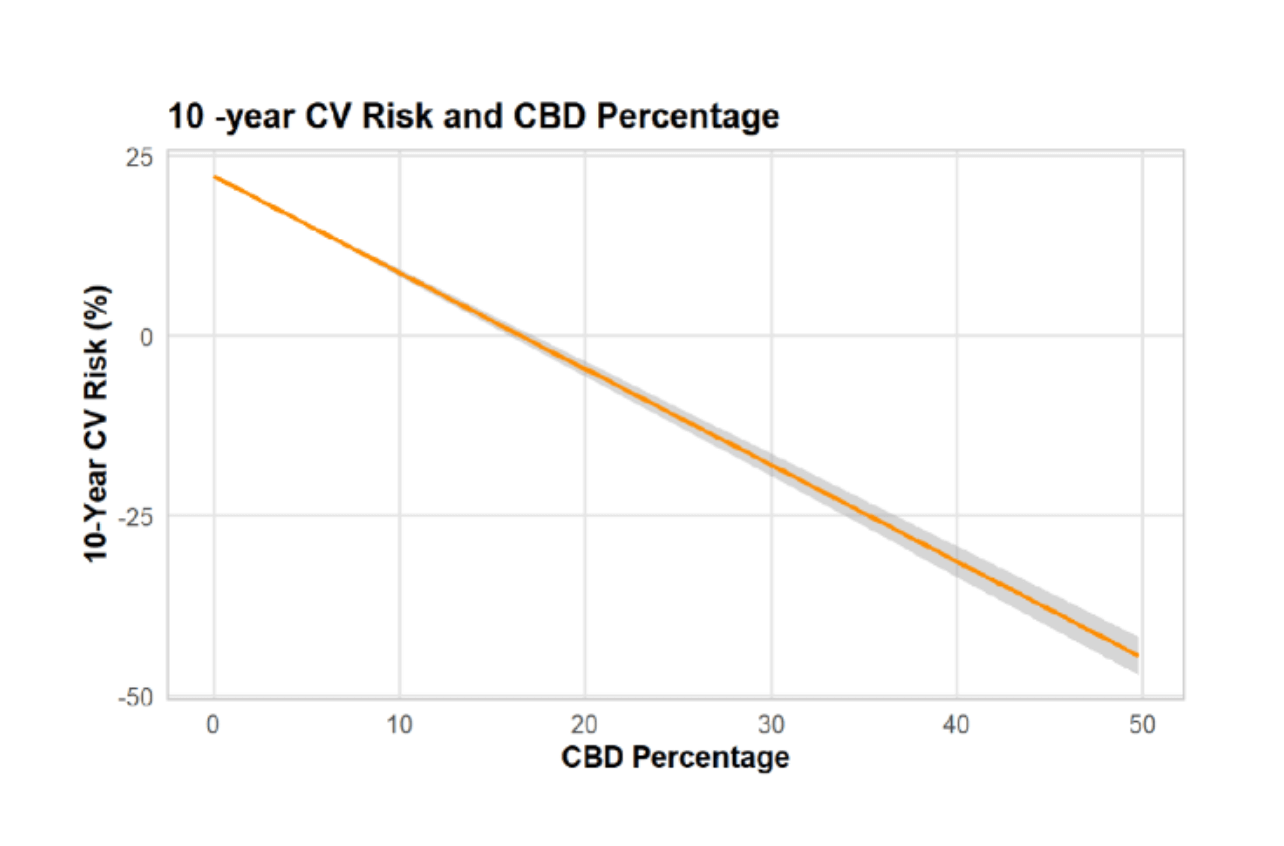
These results suggest cannabis has a complex relationship with heart health. For older adults, it may not increase near-term risk, but in younger adults, it could add to long-term concerns, and the type of product, along with the balance between THC and CBD, seems to matter.
Bottom Line
The research we have right now is enough to raise concerns, but not enough to draw firm conclusions. They should prompt thoughtful decisions, further research, and open conversations.
What To Do Now?
For patients and everyday users:
– If you use cannabis, tell your doctor what kind, how often, by what method, and how strong it seems to be. That information helps doctors better monitor your heart health.
– The pattern we see in the research is that more frequent and heavier use seems to carry more risk. It suggests that less is safer.
– How you take cannabis matters. Smoking brings added harm (carbon monoxide, fine particles). Edibles or vaping might reduce inhalation damage, but THC’s effects on the blood vessels still apply. If you smoke tobacco too, quitting or reducing it is one of the most powerful things you can do for your heart.
– Don’t ignore warning signs. Chest pain, rapid heartbeats, sudden weakness, slurred speech, or trouble breathing aren’t things to wait on. Get medical help.
For clinicians and healthcare:
– Ask patients about cannabis use as part of cardiovascular risk assessment. Document form, frequency, and estimated potency when possible.
– Stay alert to changes in cardiovascular symptoms in patients using cannabis.
– Promote and participate in research, registries, and data linkage projects.
For cannabis industry and policymakers:
– Encourage clear labeling (THC/CBD content), dosing guidance, and consumer education.
– Support partnerships to link retail sales data with health outcomes, with rigorous privacy and ethical safeguards.
– Avoid marketing ultra-potent formulations without safety data.
– Fund high-quality cardiovascular studies of cannabis use.
– Monitor trends in cannabis use and cardiovascular disease incidence in legalized jurisdictions.


Follow NCIA
Newsletter
Facebook
Twitter
LinkedIn
Instagram
–